Doses from artificial radiation are, for most of the population, much smaller than those from natural radiation but they still vary considerably. They are in principle fully controllable, unlike natural sources.
Medical. Radiation is used in medicine in two distinct ways: to diagnose disease or injury; and to kill cancerous cells. In the oldest and most common diagnostic use, X rays are passed through the patient to produce an image. The technique is so valuable that millions of X ray examinations are conducted every year. One chest X ray will give 0.1 mSv of radiation dose. For some diseases, diagnostic information can be obtained using gamma rays emitted by radioactive materials introduced into the patient by injection, or by swallowing or by inhalation. This technique is called nuclear medicine. The radioactive material is part of a pharmaceutical chosen so that it preferentially locates in the organ or part of the body being studied. To follow the distribution or flow of the radioactive material a gamma camera is used. It detects the gamma radiation and produces an image, and this indicates whether the tissue is healthy or provides information on the nature and extent of the disease.
Cancerous conditions may be treated through radiotherapy, in which beams of high energy X rays or gamma rays from cobalt-60 or similar sources are used. They are carefully aimed to kill the diseased tissue, often from several different directions to reduce the dose to surrounding healthy tissue. Radioactive substances, either as small amounts of solid material temporarily inserted into tissues or as radioactive solutions, can also be used in treating diseases, delivering high but localised radiation doses.
Medical uses of radiation are by far the largest source of man-made exposure of the public; the global yearly average dose is 0.3 millisieverts.
Environmental Radiation. Radioactive materials are also present in the atmosphere as a result of atomic bomb testing and other activities. They may lead to human exposure by several pathways external irradiation from radioactive materials deposited on the ground; inhalation of airborne radioactivity, and ingestion of radioactive materials in food and water.
Radioactive fall-out from nuclear weapons tests carried out in the atmosphere is the most widespread environmental contaminant but doses to the public have declined from the relatively high values of the early 1960s to very low levels now. The global yearly average dose is 0.006 millisieverts. However, where tests were carried out at ground level or even underground, localised contamination often remains near weapons sites.
Nuclear and other industries, and to a small degree hospitals and universities, discharge radioactive materials to the environment. Nearly all countries regulate industrial discharges and require the more significant to be authorized and monitored. Monitoring of such effluent may be carried out by the government department that authorizes the discharges as well as by the operator.
The nuclear power industry releases small quantities of a wide variety of radioactive materials at each stage in the nuclear fuel cycle. For the public the global yearly average dose is 0.008 millisieverts. The type of radioactive materials, and whether they are liquid, gaseous or particulate depends upon the operation of each process. For instance, nuclear power stations release carbon-14 and sulphur-35, which find their way through food chains to humans. Liquid discharges include radioactive materials that people may ingest through fish and shellfish.
The yearly dose to individuals living close to a power plant is small - usually a fraction of a millisievert; doses to people further away are even smaller. Reprocessing nuclear fuel produces higher doses which vary greatly from plant to plant. For the most exposed members of the public, they can be as high as 0.4 millisieverts, but for most of the population they are very much smaller.
World-wide, there are estimated to be four million workers exposed to artificial radiation as a result of their work, with an average yearly dose of about 1 millisievert. Another five million (mostly in civil aviation) have yearly average doses due to natural radiation of 1.7 millisieverts.
Non-nuclear industries also produce radioactive discharges. They include the processing of ores containing radioactive materials as well as the element for which the ore is processed. Phosphorus ores, for instance, contain radium which can find its way into the effluent. A very different industry, the generation of electricity by coal-fired power stations, results in the release of naturally-occurring radioactive materials from the coal. These are discharged to air and transfer through food chains to the population. However, the radiation doses are always low - 0.001 millisieverts or less.
Accidental releases of radioactive materials. Apart from contamination due to the normal operations of the nuclear industry, radioactivity has been widely dispersed accidentally. The most significant accident was at Chernobyl nuclear power station in the Ukraine, where an explosion caused the release of large amounts of radioactivity over a period of several days. Airborne radioactive material dispersed widely over Europe and even further afield. Contamination at ground level varied considerably, being much heavier where rain washed the radioactivity out of the air. Radiation doses therefore varied significantly from normal. More than 100,000 people were evacuated during the first three weeks following the accident. Whole body doses received from external radiation from the Ukrainian part of the 30-km exclusion zone showed an average value of 15 millisieverts. (source OECD, 1995)
Radiation in Consumer Products. Minute radiation doses are received from the artificial radioactivity in consumer goods such as smoke detectors and luminous watches, and from the natural radioactivity of gas mantles. The global yearly average dose is extremely small (0.0005 millisieverts).
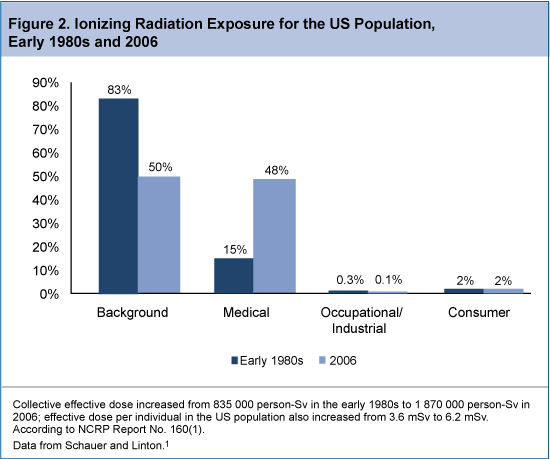 The CT technologist should be aware of the radiation risks associated with CT, and can play a leadership role in implementing tools to limit radiation exposure in patients undergoing CT imaging. Specifically, CT technologists need to understand the parameters that affect radiation dose, practice dose reduction techniques on a regular basis, and be aware of the CT examination types that are the biggest contributors to radiation exposure from CT imaging. The increased use of CT in routine clinical practice has likely resulted in a substantial increase in radiation exposure in the US population. In fact, a report from the National Council on Radiation Protection and Measurements noted as much as 7-fold increase in ionizing radiation exposure from medical procedures between the early 1980s and 2006 (Figure 2). The report estimated that in 2006, 48% of total radiation exposure was from medical procedures, as opposed to just 15% in the early 1980s.13 Among the leading contributors to the increase in CT-associated radiation exposure include imaging studies of the head, chest, abdomen/pelvis, and studies of the chest for the diagnosis of pulmonary embolism.
The CT technologist should be aware of the radiation risks associated with CT, and can play a leadership role in implementing tools to limit radiation exposure in patients undergoing CT imaging. Specifically, CT technologists need to understand the parameters that affect radiation dose, practice dose reduction techniques on a regular basis, and be aware of the CT examination types that are the biggest contributors to radiation exposure from CT imaging. The increased use of CT in routine clinical practice has likely resulted in a substantial increase in radiation exposure in the US population. In fact, a report from the National Council on Radiation Protection and Measurements noted as much as 7-fold increase in ionizing radiation exposure from medical procedures between the early 1980s and 2006 (Figure 2). The report estimated that in 2006, 48% of total radiation exposure was from medical procedures, as opposed to just 15% in the early 1980s.13 Among the leading contributors to the increase in CT-associated radiation exposure include imaging studies of the head, chest, abdomen/pelvis, and studies of the chest for the diagnosis of pulmonary embolism.



