The discussion of strategies to estimate and limit radiation dose in patients undergoing CT will require a review of the specific CT parameters that most affect radiation dose, as defined in the sections below.8
Kilovolts
Kilovolt (kV) is the amount of voltage between an X-ray tube's anode and cathode. It determines the energy of the X-ray being emitted. Higher energy X-rays have a greater potential of passing through the body and creating a signal at the detector than lower energy X-rays. Higher kV also means less noise. High-energy X-rays are absorbed by the body and deposit more energy than low-energy X-rays; therefore, contribute more to patient dose. For example, changing the kV from 120 to 135 increases the radiation dose delivered by approximately 33%. However, higher kV is sometimes warranted in larger patients or dense anatomy such as bone where increased penetration is needed.
MilliAmpere SecondsThe tube current or milliAmpere seconds (mAs) determines the number of X-rays the tube produces. Combined with the gantry rotation time, mAs represents the total X-ray output of the tube per rotation. Changing the mAs, is the most common method of adjusting dose and noise level. Cutting the mAs in half will reduce the dose by a factor of 2; however, it will also half the number of X-rays reaching the detector. Because fewer X-rays are detected, the image noise will increase and low contrast detectability will be diminished.
CT Pitch and Helical Pitch-Beam Pitch
CT pitch and helical pitch-beam pitch is defined as the distance the table travels in a rotation divided by the total active detector width in the Z direction. Helical pitch is the same except it is divided by the individual channel thickness rather than the total collimation. The higher the CT helical pitch, the faster the table moves through the X-ray beam. This results in lower radiation dose to the patient, however it may result in increased noise and may cause helical artifact. One may need to increase mAs as the pitch increases to maintain image quality.
Effective mAs Effective mAs (mAs eff) is the mAs divided by the pitch. Because pitch affects the patient dose, mAs by itself does not completely represent the number of X-rays entering the patient.
CollimationWith multislice scanning, there are many combinations of slice width and the number of slices that may be used to acquire the scan volume. With all collimators on multislice systems, the actual X-ray beam is slightly wider than the nominal beam width. This is to ensure that the detectors on the edge of the array receive uniform X-ray coverage. This results in a small amount of unused radiation. For the best image quality and dose efficiency, using the thinnest slices to cover the entire detector is ideal.
Acquired and Reconstructed Slice WidthAcquired is the actual slice thickness at which the scan was taken. Reconstructed slice width refers to post processing of the acquired slice. The acquired slice width is governed by the multislice detector configuration and determines the minimum image width that can be reconstructed. Thicker reconstructed images have less noise with all other factors being equal. However, thicker slices have less resolution. Scanning with the thinnest possible slice avoids partial volume artifacts and allows flexibility for excellent multiplanar reformats and 3-dimensional rendering without higher radiation dose. The optimal image quality and dose efficiency are achieved with the thinnest slice covering the entire detector.
Reconstruction KernelThe acquired data are filtered by the reconstruction kernel. The kernel plays a large role in determining spatial resolution. This has a great effect on the amount of noise in the image and the dose needed for a given level of image noise. There are a large variety of reconstruction kernels to select. The choice of the kernel is made based on the clinical need. Sharper reconstruction kernels are used for better in-plane spatial resolution such as in the lungs to help identify tiny airways. Smooth reconstruction kernels reduce the image noise at the expense of in-plane resolution; they are used in body imaging to reduce noise and enhance contrast resolution.
Detector Efficiency
Detector efficiency has a huge influence on the radiation dose delivered during a CT examination. The detector's ability to capture the X-ray and convert it to light, then transmit that light and convert it into an electrical signal with minimal loss, defines the overall efficiency of the detector. Better efficient detectors result in lower patient doses for a given level of image quality.
FiltrationFiltration is added outside the X-ray tube to block low-energy X-rays (photons) and reduce patient dose. The lowest energy photons will not pass through the body at all and will only contribute to patient dose. In the process of removing these low-energy photons, some desirable medium- and high-energy X-rays will be removed as well. This results in decreasing overall output of the X-ray tube. An increase in tube current or mAs may be needed to maintain image quality. A CT system needs enough filtration to block the lowest energy photons but not so much to lose the ability to distinguish low-contrast anatomy.
Patient SizeThe size of the patient plays a significant role in the total dose absorbed for the same technique. It is important to tailor the kV and mAs to the patient size to minimize the dose to the patient. With smaller patients, such as pediatric patients, the dose can be 2 to 3 times higher than on an adult. Lower kV and mAs should be used to achieve the small image quality.
Body Part Being ScannedDifferent organs in the body have different sensitivities to radiation (Table 1). For instance, the lungs are not as dense as the abdomen or pelvis because they are air filled. Therefore, less radiation (kVp and mA) is needed for imaging.
AgeThe risk of developing cancer from a CT examination decreases with increased age. Younger patients' organs are more radiosensitive in general, due to the rapid rate of cell division and growth at a young age. It is critical in young patients to keep the dose as low as possible while maintaining image quality.
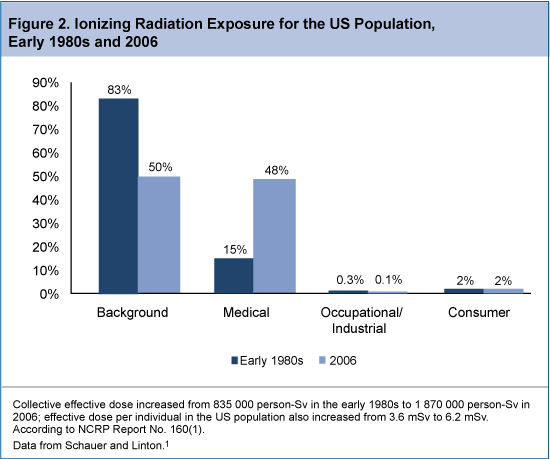 The CT technologist should be aware of the radiation risks associated with CT, and can play a leadership role in implementing tools to limit radiation exposure in patients undergoing CT imaging. Specifically, CT technologists need to understand the parameters that affect radiation dose, practice dose reduction techniques on a regular basis, and be aware of the CT examination types that are the biggest contributors to radiation exposure from CT imaging. The increased use of CT in routine clinical practice has likely resulted in a substantial increase in radiation exposure in the US population. In fact, a report from the National Council on Radiation Protection and Measurements noted as much as 7-fold increase in ionizing radiation exposure from medical procedures between the early 1980s and 2006 (Figure 2). The report estimated that in 2006, 48% of total radiation exposure was from medical procedures, as opposed to just 15% in the early 1980s.13 Among the leading contributors to the increase in CT-associated radiation exposure include imaging studies of the head, chest, abdomen/pelvis, and studies of the chest for the diagnosis of pulmonary embolism.
The CT technologist should be aware of the radiation risks associated with CT, and can play a leadership role in implementing tools to limit radiation exposure in patients undergoing CT imaging. Specifically, CT technologists need to understand the parameters that affect radiation dose, practice dose reduction techniques on a regular basis, and be aware of the CT examination types that are the biggest contributors to radiation exposure from CT imaging. The increased use of CT in routine clinical practice has likely resulted in a substantial increase in radiation exposure in the US population. In fact, a report from the National Council on Radiation Protection and Measurements noted as much as 7-fold increase in ionizing radiation exposure from medical procedures between the early 1980s and 2006 (Figure 2). The report estimated that in 2006, 48% of total radiation exposure was from medical procedures, as opposed to just 15% in the early 1980s.13 Among the leading contributors to the increase in CT-associated radiation exposure include imaging studies of the head, chest, abdomen/pelvis, and studies of the chest for the diagnosis of pulmonary embolism.
